Step Three: Planning
Purpose: to assist in planning client care that is individualized, realistic, measurable, and which promotes patient participation and involvement of support people. If the plan of care we develop is successful, then our expected outcome will be met.
- Setting Priorities
- Setting Goals & Outcomes
- Developing the Plan of Care
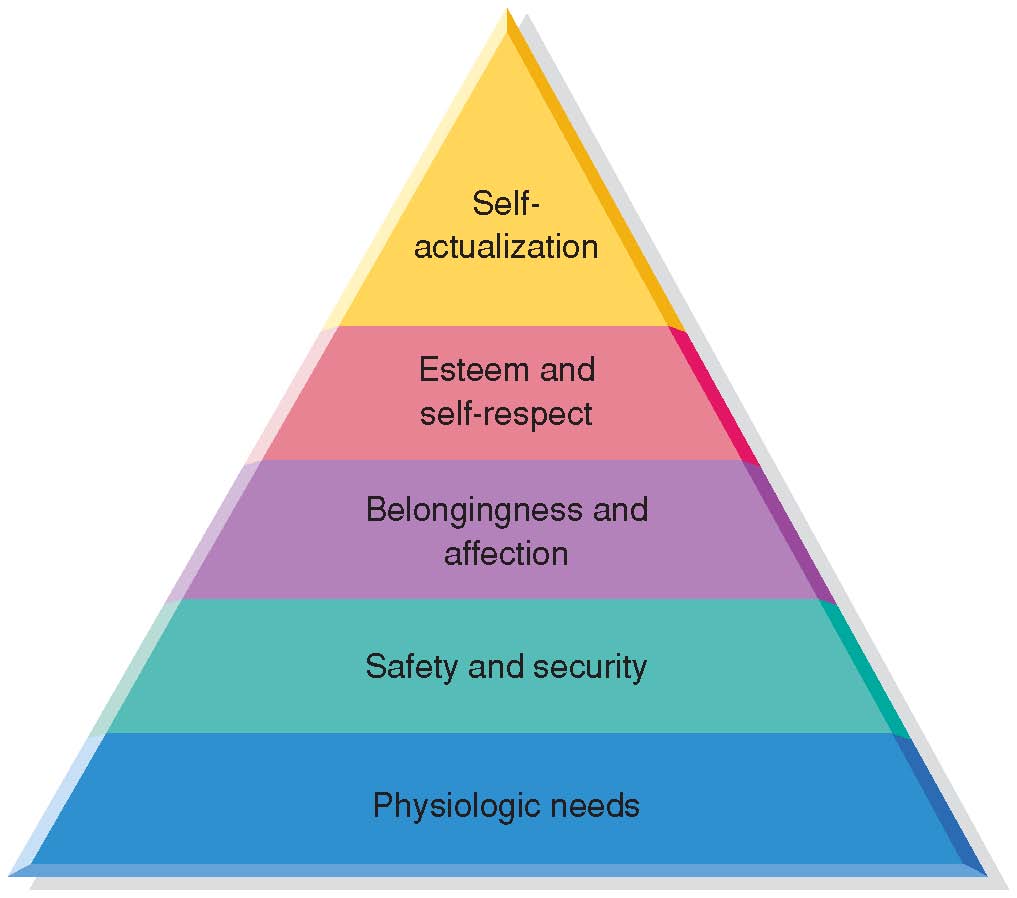
Maslow's Heierarchy of Needs
Abraham Maslow’s Human Needs Theory (1968) places human needs into a hierarchy of motivation. All needs are steps toward self actualization. According to Maslow, a person must meet their basic (often physiologic) needs in order to step up to the next level. Nurses must prioritize their patient’s needs from the bottom up, and provide appropriate care that is individualized and based on mutually agreed upon goals. The patient is an active part of the planning process.

